JOINTS 2023;
1: e812
DOI: 10.26355/joints_202312_812
Does the number of screws to fix scarf osteotomy influence the radiographic outcome and the complication rate in hallux valgus? A proportional meta-analysis and systematic review
Topic: Current concepts
Category: Systematic Review
Abstract
OBJECTIVE: Scarf osteotomy is a midshaft osteotomy of the first metatarsal, which is commonly adopted to treat moderate to severe hallux valgus (HV) deformity. Our aim was to determine whether the number of screws used to fix a Scarf osteotomy in the treatment of HV might influence the radiographic correction achieved, the complication, and the recurrence rate at the longest possible follow-up.
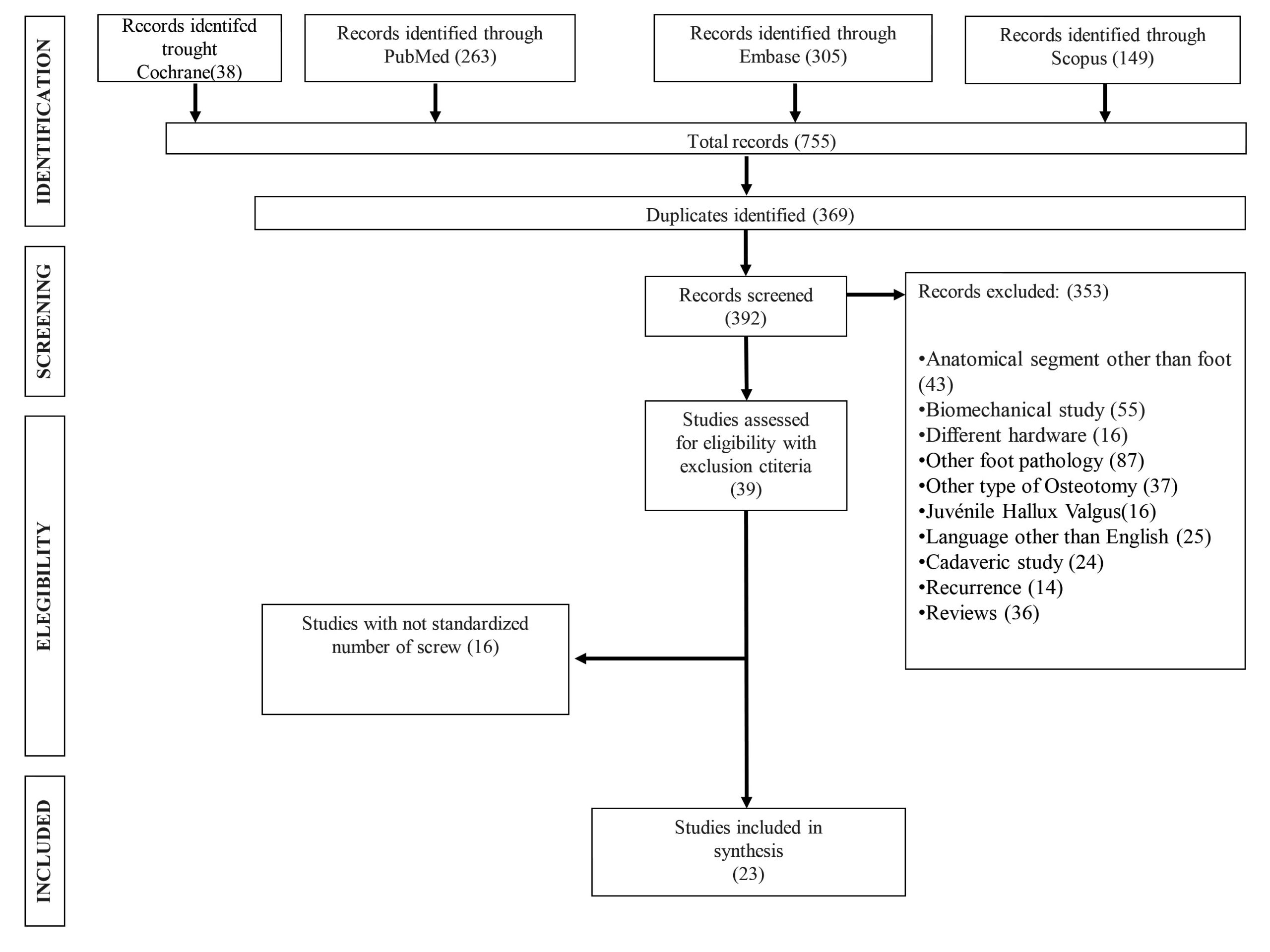
MATERIALS AND METHODS: This PROSPERO-registered systematic review followed the PRISMA statement. Using multiple databases (PubMed, Embase, Cochrane Library, and Scopus), we selected all clinical studies dealing with open scarf osteotomy to treat HV in skeletally-mature patients. Data were harvested regarding the cohort, the study design, the surgical technique, and the clinical and radiographic outcomes. Three groups were built based on the type of fixation [screwless Scarf osteotomy (0S), Scarf osteotomy fixed with a single screw (1S) or with two screws (2S)] and compared. The risk of bias was assessed using the ‘non-randomized studies-of intervention’ (ROBINS-I) tool.
RESULTS: Twenty-eight series of patients from twenty-three studies (1,964 feet) were selected (G1=259 ankles, G2=391, G3=1,314). The overall median follow-up was 24.5 months (IQR, 24-36), but it was longer for 1S (median 64.9 months; IQR, 34-109) as compared to 0S (median 20 months; IQR, 16-84) and 2S (median 24 months; IQR, 24-26) (p=0.04). Pre- and post-operative HVA (Hallux Valgus angle) and IMA (Intermetatarsal Angle) angles, as long as the mean improvement after surgery for both angles (for HVA, 0S: 22.4° vs. 1S: 17.5° vs. 2S: 20.8°; p=0.14; for IMA, 0S: 8.4° vs. 1S: 5.9° vs. 2S: 6.6°; p=0.42) were not different. The pooled proportion estimate showed a similar complication rate in the three groups [0S: 14% (95% CI, 0-30); 1S: 13% (95% CI, 1-26); 2S: 13% (95% CI, 6-16)]. When comparing the pooled complication rate in the screwless group and in the fixed-with-screws group, the difference was not significant either [0S: 14% (95% CI, 0-30); 1S+2S: 13% (95% CI, 9-17); p=0.97]. The pooled proportion of recurrence was similar in the three groups as well [0S: 2% (95% CI, 0-3); 1S: 9% (95% CI, 0-17); 2S: 3% (95% CI, 2-5)]. When comparing the pooled recurrence rate in the screwless group and in the fixed-with-screws one, the difference was not significant [0S: 2% (95% CI, 0-3); 1S+2S: 4% (95% CI, 2-5); 95% CI p=0.55]. The risk of bias was low, moderate, and serious in 2, 18, and 3 studies, respectively.
CONCLUSIONS: This systematic review suggested that the radiographic correction achieved using a screwless Scarf, a single-screw technique, and a traditional two-screw procedure is not significantly different. At a median 2-year follow-up, the complication and the recurrence rates were not different either.
Introduction
Scarf osteotomy is a midshaft osteotomy of the first metatarsal, which is commonly adopted to treat moderate to severe hallux valgus (HV) deformity1-3. After its original description in 1989 by Zygmunt et al4, multiple studies5-9 have been led documenting satisfactory results in terms of clinical outcome, radiographic correction, patient satisfaction5-7, and complication rate (which stands at 6-11%, according to some recent reviews8,9). While the technique was initially performed using two cannulated screws (a distal one in the distal meta-epiphysis to stabilize the metatarsal head and a proximal one in the shaft to achieve a greater contact area and to avoid rotational instability), some authors have proposed the use of a single (distal) screw claiming that this could be sufficient in order to obtain sufficient stability of the osteotomy10-12. Moreover, Besse and Maestro12 have recently described a screwless fixation technique for scarf osteotomy, whereby a second small cut in the inner distal corner of the proximal fragment would create a step to accommodate the metatarsal head and keep both fragments in contact throughout the healing process and without metalwork. While a greater number of screws would ideally help increase the stability at the expense of an increased risk of metalwork-related complications (i.e., breakage during use, soft tissue irritation at the tip or at the head of the screw, potential need to re-operate to remove the hardware), to the best of our knowledge, no comparative study has been conducted so far to demonstrate which fixation method might be actually superior.
With this background, we have performed a systematic review aimed at determining whether the number of screws used to fix scarf osteotomy in the treatment of HV might influence the radiographic correction achieved, the complication rate, and the recurrence rate at the longest possible follow-up. We hypothesized that a greater number of screws might be related to increased stability in the short-term (with improved radiographic correction) but with a higher complication rate in the long run (related to the presence of metalwork).
Materials and Methods
Study Design
This systematic review was designed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA, Supplementary Figure 1)13. It was prospectively registered in the PROSPERO database (CRD42023430426). As a review, no ethical approval or informed consent was requested for this study.
Eligibility Criteria
To be included in this review, studies had to meet the following criteria: studies reporting data after open Scarf osteotomy for HV stabilized using either two screws, either one screw or no metalwork, in patients aged between 18 and 85 years; a clear description of the surgical technique with one or more statements regarding the number of screws used; studies including a sample size larger than 10 feet; assessment of radiographic results through pre- and post-operative weight-bearing standardized radiographs; studies reporting the clinical results, complications, and re-operations after scarf osteotomy; minimum follow-up of 12 months; randomized, quasi-randomized, prospective and retrospective cohort studies, case series, technical notes; studies published in any language; full-text availability either online either after direct contact with the authors.
Exclusion criteria were as follows: studies reporting results after scarf osteotomy stabilized using other methods or performed percutaneously; studies in which screws were used as a unique fixation strategy but a variable number of screws within the same cohort; data on skeletally-immature patients; case reports, biomechanical studies, cadaveric studies, expert opinions, letters to the editor, studies on animals and instructional courses. Narrative or systematic reviews were also excluded from the study, but references were double-checked in order to identify potentially eligible studies.
Information Sources and Search
A systematic search was conducted on PubMed, Embase, Cochrane Library, and Scopus, from the earliest entries through May 10, 2023, with the following keywords and Boolean operators: ((scarf) AND (osteotomy*)) AND ((hallux) AND (valgus)). Two reviewers (AI and GM) independently screened the results of the research, and then the full text of eligible studies was analyzed. Disputes were resolved by the senior author after discussion (AB). Unpublished studies and gray literature were not considered.
Data Charting and Items
Data were charted independently by two investigators (AI and GM) using an Excel sheet. Data were harvested regarding the cohort, the study design, the surgical technique, clinical results, and the complication rate at the longest follow-up. Results were compared in order to verify that no data were missed. Three groups were built based on the type of fixation adopted: screwless scarf osteotomy (0S), scarf osteotomy fixed with a single screw (1S) or with two screws (2S).
Risk of Bias
The risk of bias for studies included in this review was assessed using the ‘non-randomized studies-of intervention’ (ROBINS-I) tool14. This allowed the evaluation of a pre-intervention bias (due to confounding and participant selection), an at-intervention bias (classification of intervention), and a post-intervention bias (deviations, missing data, measurement of outcomes, reported results). According to this score, studies were classified as low risk, moderate risk, severe risk, and critical risk. Two investigators performed the ROBINS-I assessment twice (AI and GM) at an interval of 10 days, then discussed the scores when the difference was present until a consensus was reached.
Statistical Analysis
Values were reported as mean, standard deviation, or 95% confidence interval [95% CI] and ranges (minimum and maximum values) for normally distributed variables and as medians and interquartile ranges (IQR) for nonnormally distributed variables. The normality of data was assessed using the Shapiro-Wilk test. Baseline characteristics and the improvement in radiographic angles in the three groups (0S vs. 1S vs. 2S) were compared using the analysis of variance (ANOVA) test with the Bonferroni correction (B) of p-value or the Kruskal-Wallis’ test followed by the Dunn’s pairwise comparison (depending on the distribution of data). The Chi-squared test was used for categorical variables. A proportional meta-analysis was run to pool data regarding the rate of complication and recurrence in the screwless (0S) and with-screws group (1S + 2S). The ‘metaprop’ command was used to compute 95% CI using the score statistic and the exact binomial method and incorporate the Freeman-Tukey double arcsine transformation of proportions. Heterogeneity among studies was assessed through the Higgins’ I² statistic, and a random-effect model was applied in all cases. STATA statistical software package (version 12.0, StataCorp, College Station, TX, USA) was used for statistical analysis. A p-value significance level was set at 0.05.
Results
Twenty-eight series of patients from twenty-three studies (1964 feet) were selected (G1=259 ankles15-17, G2=39118-21, G3=131422-37) (Table 1, Figure 1).
Table 1. Main characteristics of studies included in this review.
| Author (year) | Study design | LoE | Akin procedure (Y/N) | Soft tissue procedures
(Y/N) |
ROBINS-I
overall risk of bias |
| Screwless scarf | |||||
| Leemrijse et al15 (2012) | Retr – Non Comp | IV | No | Yes | Moderate |
| Curtin et al16 (2018) | Retr – Non Comp | IV | Yes | Yes | Moderate |
| Rouveyrol et al17 (2021) | Retr – Non Comp | IV | Yes | Yes | Moderate |
| Single-screw scarf | |||||
| Kristen et al18 (2002) | Retr – Non Comp | IV | Yes | Yes | Moderate |
| De Vil et al19 (2010) | Prosp – Comp | II | No | Yes | Moderate |
| Bock et al20 (2015) | Retr – Non Comp | IV | Yes | Yes | Moderate |
| Rajeev21 (2019) | Retr – Non Comp | IV | Yes | Yes | Moderate |
| Two-screw scarf | |||||
| Creivoisier et al22 (2001) | Retr – Non Comp | IV | Yes | Yes | Moderate |
| Jones et al23 (2004) | Prosp – Non Comp | II | Yes | Yes | Moderate |
| Garrido et al24 (2007) | Retr – Non Comp | IV | Yes | Yes | Moderate |
| Gupta et al25 (2008) | Retr – Non Comp | IV | Yes | Yes | Moderate |
| Furhmann et al26 (2009) | Retr – Non Comp | IV | Yes | Yes | Serious |
| Paczesny et al27 (2009) | Retr – Non Comp | IV | Yes | Yes | Serious |
| Murawski et al28 (2010) | Retr – Non Comp | IV | Yes | Yes | Serious |
| Choi et al30 (2013) | Retr – Non Comp | IV | Yes | Yes | Moderate |
| Deveci et al31 (2013) | Retr – Non Comp | III | Yes | Yes | Moderate |
| Marudanayagam32 (2014) | Retr – Non Comp | IV | Yes | Yes | Moderate |
| Milczarek et al29 (2017) | Prosp – Non Comp | II | No | Yes | Moderate |
| Boychenko et al33 (2018) | Prosp – Comp | I | Yes | Yes | Low |
| Samaras et al34 (2019) | Retr – Non comp | III | Yes | Yes | Moderate |
| Law et al35 (2020) | Retr – Comp | III | Yes | Yes | Moderate |
| Veracruz-Galvez et al36 (2022) | Prosp – Comp | II | Yes | Yes | Low |
| Xie et al37 (2022) | Retr – Non Comp | IV | Yes | Yes | Moderate |
Prosp, Prospective; Retr, Retrospective; Comp, Comparative; Non Comp, Non Comparative; LoE, Level of Evidence; Y, Yes; N, No.
Figure 1. Flow chart PRISMA 2020 model for studies included in this systematic review.
At baseline, the three groups were comparable by number of patients (p=0.55), number of feet (p=0.40), percentage of female patients (p=0.72), age of patients (p=0.20), pre-operative AOFAS score (0.73) and pre-operative radiographic angles (HVA, p=0.94; IMA, p=0.08). The overall median follow-up was 24.5 months (IQR, 24-36), but it was longer in 1S (median 64.9 months; IQR, 34-109) as compared to 0S (median 20 months; IQR, 16-84) and 2S (median 24 months; IQR, 24-26) (p=0.04, Table 2).
Table 2. Baseline demographics, follow-up, and clinical status (AOFAS score) of the cohorts investigated in the studies included in this review.
| Screwless scarf | Single-screw scarf | Two-screw scarf | |||||||||
| Median and IQR 25-75%*
or Mean and 95% CI** |
Range | Median and IQR 25-75%*
or Mean and 95% CI** |
Range
|
Median and IQR 25-75%*
or Mean and 95% CI** |
Range
|
||||||
| Patients (N)* | 76 | 12-148 | 12-148 | 91 | 55-114.5 | 21-136 | 49.5 | 30-71 | 17-162 | ||
| Feet (N)* | 96 | 15-148 | 15-148 | 102 | 57-138.5 | 21-166 | 53 | 37-72 | 11-199 | ||
| Sex (% F)** | 0.88 | 0.84-0.91 | 0.83-0.92 | 0.81 | 0.68-0.84 | 0.73-0.91 | 0.9 | 0.78-0.91 | 0.72-1 | ||
| Mean age (y)** | 55.3 | 54.5-56.3 | 54-57 | 52.4 | 48.2-54 | 45-59.8 | 51.9 | 48.3-60 | 40-62 | ||
| Mean follow-up (m)* | 20 | 16-84 | 16-84 | 64.9 | 34.4-109.5 | 34-124 | 24 | 24-26 | 18-45 | ||
| Pre-operative AOFAS score (points)** | 51 | NA | 50-51 | 52.8 | NA | 47-57 | 44.4 | NA | 35-52 | ||
IQR, interquartile range; 95% CI, 95% Confidence Interval; N, number; F, female; y, years; m, months; AOFAS, American Orthopaedic Foot and Ankle Society; NA, not available because of lack of raw data in primary studies.
Improvement in Radiographic Angles
Pre- and post-operative HVA and IMA angles in the three groups have been outlined in Table 3. The mean improvement both for HVA [0 S: 22.4° (95% CI, 15.3-29.5); 1S: 17.5° (95% CI, 15.8-19.3); 2S: 20.8° (95% CI, 18.2-23.4); p=0.14] and IMA [0S: 8.4° (95% CI, 6.1-10.7); 1S: 5.9° (95% CI, 4.8-7); 2S: 6.6° (95% CI, 5.6-7.6); p=0.42] was similar in 0S, 1S and 2S.
Table 3. Pre- and post-operative radiographic values extracted from the cohorts included in this review.
| Screwless scarf | Single-screw scarf | Two-screw scarf | |||||||
| Median | IQR 25-75% | Range | Median | IQR 25-75% | Range | Median | IQR 25-75% | Range | |
| Pre-operative HVA | 35 | 28.1-38.5 | 27-39 | 31.8 | 29.5-35.7 | 27.9-39 | 36 | 33-38.1 | 16.7-44.2 |
| Post-operative HVA | 11.5 | 10.6-12.1 | 10-13 | 14.2 | 12.6-17.5 | 11.8-20 | 13.6 | 12-15-2 | 5.1-26.3 |
| Pre-operative IMA | 15 | 13.1-15.1 | 12-16 | 14.2 | 13.9-14.7 | 13.5-15 | 14.7 | 13.6-16 | 11.1-19.1 |
| Post-operative IMA | 4.8 | 4.3-8.7 | 4-8.9 | 8.5 | 7.5-9.3 | 7-9.6 | 8.6 | 6.8-9.1 | 4.2-10.7 |
| Mean | 95% CI | Range | Mean | 95% CI | Range | Mean | 95% CI | Range | |
| Difference for HVA
(pre vs. post) |
22.4 | 15.3-29.5 | 15-30 | 17.5 | 15.8-19.3 | 15-19.8 | 20.8 | 18.2-23.4 | 9.1-32.1 |
| Difference for IMA
(pre vs. post) |
8.4 | 6.1-10.7 | 6-11 | 5.9 | 4.8 – 7 | 4.4-7.1 | 6.6 | 5.6-7.6 | 3.1-10.4 |
IQR, interquartile range; 95% CI, 95% Confidence Interval; HVA, Hallux Valgus Angle; IMA, Inter Metatarsal Angle.
Pooled Estimate of Complication and Recurrence Rate
A list of complications (including recurrence) after scarf osteotomy, extracted from studies included in this review, has been reported in Supplementary Table 1. The pooled proportion estimate showed a similar complication rate in the three groups [0S: 14% (95% CI, 0-30); 1S: 13% (95% CI, 1-26); 2S: 13% (95% CI, 6-16)] (Figure 2). When comparing the pooled complication rate in the screwless group and in the fixed-with-screws one, the difference was not significant [0S: 14% (95% CI, 0-30); 1S+2S: 13% (95% CI, 9-17); p=0.97]. The intergroup statistical heterogeneity was nonsignificant (p=0.936) (Figure 3).
Figure 2. Meta-analysis of the proportion of complications in patients who underwent scarf osteotomy for hallux valgus deformity fixed using three methods (no screws, 1 screw, and 2 screws). Output generated by the Stata procedure metaprop.

Figure 3. Meta-analysis of the proportion of complications in patients who underwent scarf osteotomy for hallux valgus deformity using a screwless technique vs. a with-screws (1 or 2) technique. Output generated by the Stata procedure metaprop.

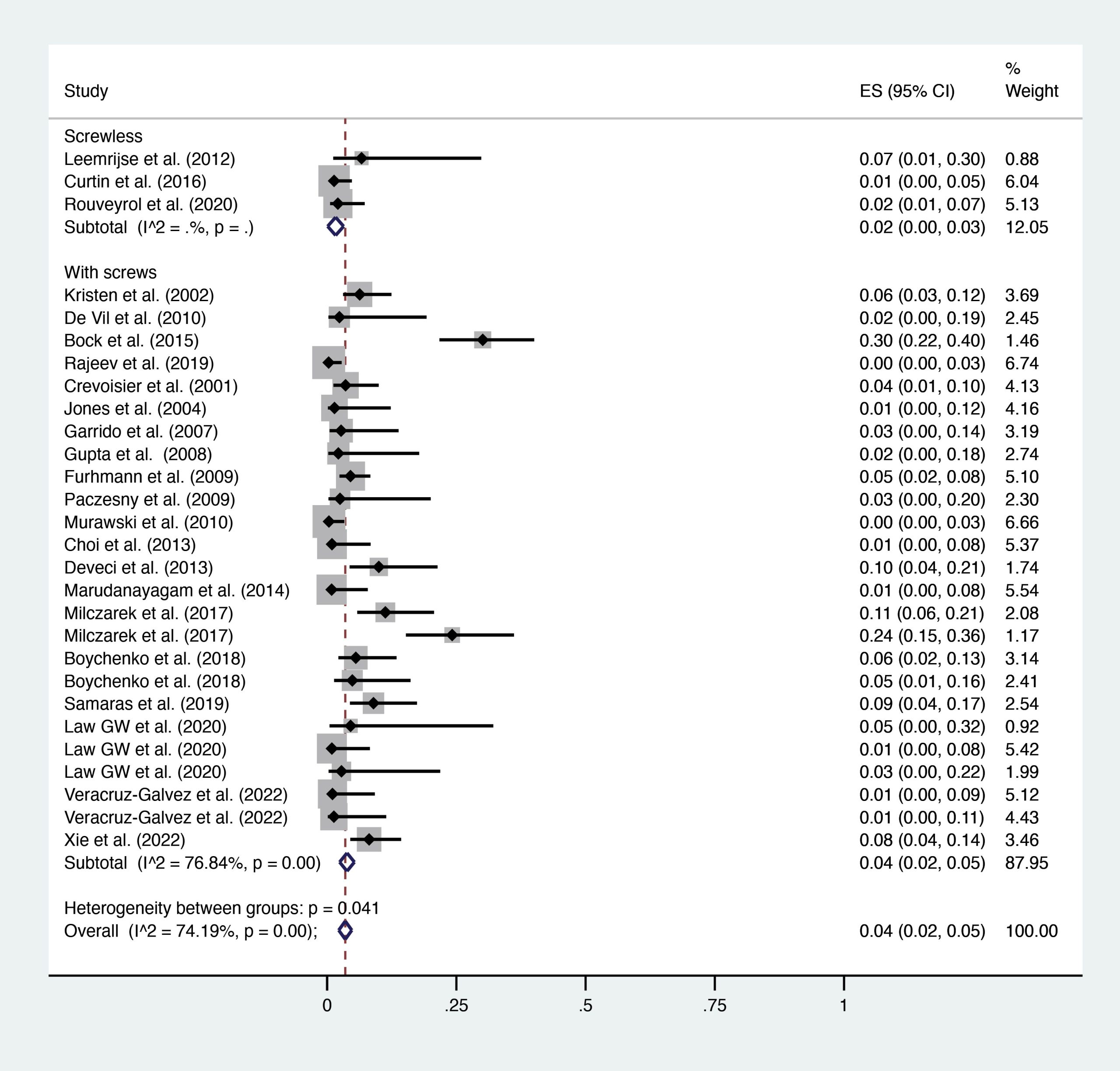
The pooled proportion of recurrence was similar in the three groups as well [0S: 2% (95% CI, 0-3); 1S: 9% (95% CI, 0-17); 2S: 3% (95% CI, 2-5)] (Figure 4). When comparing the pooled recurrence rate in the screwless group and in the fixed-with-screws one, the difference was not significant either [0S: 2% (95% CI, 0-3); 1S+2S: 4% (95% CI, 2-5); p=0.55] (Figure 5). There was a significant statistical heterogeneity between groups for the overall recurrence rate analysis (p=0.041) (Figure 5).
Figure 4. Meta-analysis of the proportion of recurrence in patients who underwent scarf osteotomy for hallux valgus deformity fixed using three methods (no screws, 1 screw, and 2 screws). Output generated by the Stata procedure metaprop.

Figure 5. Meta-analysis of the proportion of recurrence in patients who underwent scarf osteotomy for hallux valgus deformity using a screwless technique vs. a with-screws (1 or 2) technique. Output generated by the Stata procedure metaprop.
Risk of Bias
The risk of bias was low, moderate, and serious in 233,36, 1815-25,29-32,34,35,37, and 3 studies26-28, respectively (Table 1).
Discussion
The main finding of this study was that the number of screws used to stabilize a scarf osteotomy in the treatment of HV did not seem related to the degree of correction achieved at the end of the procedure, which was assessed through traditional radiographic angles, nor to the risk of complication or recurrence in the short-term. More in detail, our analysis revealed a pooled complication rate standing at approximately 13-14%, regardless of the fixation method chosen. The recurrence rate stood at 2-3% for screwless and two-screw osteotomies, against an unexpected 9% for single-screw osteotomies. While the difference was statistically non-significant, we reckon that the apparent greater risk of recurrence when using a single screw might be consequential to biases related to the longer follow-up in studies reporting this type of fixation (median value over 5 years) as compared to the other two methods (median value around 2 years). In particular, this was the result of a very long follow-up reported in two out of four studies in the 1S group, i.e., De Vil et al19 (mean: 95 months) and Bock et al20 (mean: 124 months).
Regarding the radiographic analysis, this could only be performed by assessing the HVA and the IMA since other measurements [such as the distal metatarsal articular angle (DMAA) or the sesamoid position] were not regularly reported in primary studies included in this review (Table 2). Overall, the results confirmed that scarf osteotomy is not inferior to other surgical techniques in the correction of moderate-to-severe HV6,38,39. Although the median value for HVA and IMA was quite similar in the three groups, at least two considerations have to be made. First, it should be considered that the number of studies in the screwless and in the single-screw group were way lower than the number of studies in which the traditional fixation using two screws had been adopted. While studies in literature were comparable in terms of baseline characteristics, as shown above, this discrepancy could let us hypothesize that less positive results obtained through the screwless and one-screw technique might not have been shared in scientific publications. This is particularly supported by the inherent difficulty of performing a screwless technique, which has been defined as ‘effective but technically demanding’ by authors like Curtin et al16. Second, even if the original scarf technique allowed the shift of the metatarsal head up to one-third of the metatarsal width (in order to keep sufficient contact among surfaces, to improve stability, and to increase the chances of healing), some surgeons have often dared to push the limits of the technique until only a cortical contact was kept, shifting the distal fragment by approximately 95% of the bone width. Considering the instability coming from such displacement, some metalwork would certainly be required in order to achieve sufficient stability between the two fragments. It appears reasonable to think that, in such extreme cases, this degree of correction would not be achievable using the screwless technique since the risk of instability would probably be too high. On the other side, it is true that only a prospective comparative study on severe HV might shed more light in this area and clarify whether the non-fixed scarf might have some ‘limited’ indications as compared to the traditional one.
For what concerns the complication and the recurrence rates, the pooled analysis did not show any significant difference in the three groups. However, looking at complications reported in each study (Supplementary Table 1), it should be highlighted that ‘hardware-related pain’ has been reported in 822,23,26,28,30,34,35,37 out of 21 cohorts (38%) of the two-screw group, ranging from 0.5% to 7.5% of cases. This confirms that, during the pre-operative counseling for a traditional scarf osteotomy, the possibility of issues coming from screws should be thoroughly discussed with patients. On the other hand, in the screwless group, we would have expected a higher rate of loss of correction or non-union, which conversely were both reported only in 1-1.5% of cases15. Regarding the recurrence rate, as explained above, we believe that further studies on the screwless and one-screw techniques are warranted in order to balance the length of follow-up in a theoretical comparative analysis before drawing any reliable conclusion. However, it is worth underlining that only 3 studies20,31,33 in this review provided with a clear definition of recurrence throughout the text. The review published by Clarke and Platt9 found a recurrence rate after scarf osteotomy at 3.6-11%, clarifying how this result is usually strongly affected both by the definition adopted by authors and by the length of follow-up. To date, and to the best of our knowledge, there is still no unanimous consensus in the literature about the radiographic and/or clinical definition of recurrence, which makes any comparison in this area even harder.
Limitations
The authors acknowledge some limitations of this study. First, the inclusion of Level III and IV studies, which are by definition not prospective and, therefore, potentially biased in their results. Our choice was dictated by both the intention to include a greater number of studies dealing with scarf osteotomy and the lack of high-quality specific analyses in the field. Nevertheless, in the absence of primary comparative studies, the extraction of dichotomous variables allowed us to run an appropriate statistical analysis and calculate the pooled proportion estimate for recurrence and postoperative complication rate, which strengthens our findings. Third, although the statistical heterogeneity found in the comparison of the three groups was nonsignificant, some inevitable heterogeneity coming from the comparison of studies from different authors must be kept in mind, since they may still differ in some aspects of the treatment proposed to the patient (i.e., type of screw, the position of the screw, postoperative protocol). Last, the difference in terms of follow-up between the 1S group and the other two groups should be considered a potential additional source of bias when evaluating our results.
Conclusions
This systematic review suggested that the radiographic correction achieved using a screwless scarf, a single-screw technique, and a traditional two-screw procedure in HV are not significantly different. At a median 2-year follow-up, the complication rate and the recurrence rate were not different either. Prospective studies comparing different fixation methods at a longer follow-up are required in order to determine which method leads to the best clinical outcome.
Conflict of Interest
The authors declare no conflict of interest directly or indirectly related to this work.
Funding
No funding has been provided for the current work.
Informed Consent
Not applicable.
Ethics Approval
Not applicable.
ORCID ID
Antonio Izzo: 0000-0001-5018-3835
Giovanni Manzi: 0000-0003-1722-3019
Massimo Mariconda: 0000-0002-9906-5124
Alessio Bernasconi: 0000-0002-9427-3178
References
- Trnka HJ. Osteotomies for hallux valgus correction. Foot Ankle Clin 2005; 10: 15-33.
- Boksh K, Qasim S, Khan K, Tomlinson C, Mangwani J. A Comparative Study of Mini-Scarf Versus Standard Scarf Osteotomy for Hallux Valgus Correction. J Foot Ankle Surg 2018; 57: 948-951
- Coetzee JC, Rippstein P. Surgical strategies: scarf osteotomy for hallux valgus. Foot Ankle Int 2007; 28: 529-535.
- Zygmunt KH, Gudas CJ, Laros GS. Z-bunionectomy with internal screw fixation. J Am Podiatr Med Assoc 1989; 79: 322-329.
- Deng W, Chen Y, Li YX, Wu SZ, Ren Y, Huang FG, Zhang H. [Chevron osteotomy versus Scarf osteotomy for the efficacy of radiographic and clinical in moderate and severe hallux valgus:a systematic review]. Zhongguo Gu Shang 2019; 32: 765-771.
- Fukushi JI, Tanaka H, Nishiyama T, Hirao M, Kubota M, Kakihana M, Nozawa D, Watanabe K, Okuda R. Comparison of outcomes of different osteotomy sites for hallux valgus: A systematic review and meta-analysis. J Orthop Surg (Hong Kong) 2022; 30: 10225536221110473.
- Matar HE, Platt SR. Overview of randomised controlled trials in hallux valgus surgery (2,184 patients). Foot Ankle Surg 2021; 27: 351356.
- Sieloff MR, Tokarski AR, Elliott AD, Jacobs PM, Borgert AJ. The Incidence of Complications Following Scarf Osteotomy for the Treatment of Hallux Valgus: A Systematic Review With Meta-Analysis. J Foot Ankle Surg 2023; 62: 610-617.
- Clarke TAC, Platt SR. Treatment of hallux valgus by Scarf osteotomy – rates and reasons for recurrence and rates of avascular necrosis: A systematic review. Foot Ankle Surg 2021; 27: 622-628.
- Ma Q, Liang X, Lu J. Chevron osteotomy versus scarf osteotomy for hallux valgus correction: A meta-analysis. Foot Ankle Surg 2019; 25: 755-760.
- Kramer J, Barry LD, Helfman DN, Mehnert JA, Pokrifcak VM. The modified Scarf bunionectomy. J Foot Surg 1992; 31: 360-367.
- Besse JL, Maestro M. Ostéotomies SCARF du 1er métatarsien [First metatarsal SCARF osteotomies]. Rev Chir Orthop Reparatrice Appar Mot 2007; 93: 515-523.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71.
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016; 355: i4919.
- Leemrijse T, Maestro M, Tribak K, Gombault V, Devos Bevernage B, Deleu PA. Scarf osteotomy without internal fixation to correct hallux valgus. Orthop Traumatol Surg Res 2012; 98: 921-927.
- Curtin M, Murphy E, Bryan C, Moroney P. Scarf osteotomy without internal fixation for correction of hallux valgus: A clinical and radiographic review of 148 cases. Foot Ankle Surg 2018; 24: 252-258.
- Rouveyrol M, Harrosch S, Curvale G, Rochwerger A, Mattei JC. Does screwless scarf osteotomy for hallux valgus increase the risk of transfer metatarsalgia? Orthop Traumatol Surg Res 2021; 107: 102853.
- Kristen KH, Berger C, Stelzig S, Thalhammer E, Posch M, Engel A. The SCARF osteotomy for the correction of hallux valgus deformities. Foot Ankle Int 2002; 23: 221-229.
- De Vil JJ, Van Seymortier P, Bongaerts W, De Roo PJ, Boone B, Verdonk R. Scarf osteotomy for hallux valgus deformity: a prospective study with 8 years of clinical and radiologic follow-up. J Am Podiatr Med Assoc 2010; 100: 35-40.
- Bock P, Kluger R, Kristen KH, Mittlböck M, Schuh R, Trnka HJ. The Scarf Osteotomy with Minimally Invasive Lateral Release for Treatment of Hallux Valgus Deformity: Intermediate and Long-Term Results. J Bone Joint Surg Am 2015; 97: 1238-1245.
- Rajeev A, Tumia N. Three-Year Follow-Up Results of Combined Short Scarf Osteotomy With Akin Procedure for Hallux Valgus. J Foot Ankle Surg 2019; 58: 837-841.
- Crevoisier X, Mouhsine E, Ortolano V, Udin B, Dutoit M. The scarf osteotomy for the treatment of hallux valgus deformity: a review of 84 cases. Foot Ankle Int 2001; 22: 970-976.
- Jones S, Al Hussainy HA, Ali F, Betts RP, Flowers MJ. Scarf osteotomy for hallux valgus. A prospective clinical and pedobarographic study. J Bone Joint Surg Br 2004; 86: 830-836.
- Garrido IM, Rubio ER, Bosch MN, González MS, Paz GB, Llabrés AJ. Scarf and Akin osteotomies for moderate and severe hallux valgus: clinical and radiographic results. Foot Ankle Surg 2008; 14: 194-203.
- Gupta S, Fazal MA, Williams L. Minifragment screw fixation of the Scarf osteotomy. Foot Ankle Int 2008; 29: 385-389.
- Fuhrmann RA, Zollinger-Kies H, Kundert HP. Mid-term results of Scarf osteotomy in hallux valgus. Int Orthop 2010; 34: 981-989.
- Paczesny L, Kruczyński J, Adamski R. Scarf versus proximal closing wedge osteotomy in hallux valgus treatment. Arch Orthop Trauma Surg 2009; 129: 1347-1352.
- Murawski CD, Egan CJ, Kennedy JG. A rotational scarf osteotomy decreases troughing when treating hallux valgus. Clin Orthop Relat Res 2011; 469: 847-853.
- Milczarek MA, Milczarek JJ, Tomasik B, Łaganowski P, Nowak K, Domżalski M. Being overweight has limited effect on SCARF osteotomy outcome for hallux valgus correction. Int Orthop 2017; 41: 765-772.
- Choi JH, Zide JR, Coleman SC, Brodsky JW. Prospective study of the treatment of adult primary hallux valgus with scarf osteotomy and soft tissue realignment. Foot Ankle Int 2013; 34: 684-690.
- Deveci A, Firat A, Yilmaz S, Oken OF, Yildirim AO, Ucaner A, Bozkurt M. Short-term clinical and radiologic results of the scarf osteotomy: what factors contribute to recurrence? J Foot Ankle Surg 2013; 52: 771-775.
- Marudanayagam A, Appan SV. Scarf osteotomy with or without proximal phalangeal osteotomy for severe hallux valgus deformity. J Orthop Surg (Hong Kong) 2014; 22: 39-41.
- Boychenko AV, Solomin LN, Belokrylova MS, Tyulkin EO, Davidov DV, Krutko DM. Hallux Valgus Correction With Rotational Scarf Combined With Adductor Hallucis Tendon Transposition. J Foot Ankle Surg 2019; 58: 34-37.
- Samaras D, Gougoulias N, Varitimidis S, Hantes M, Karachalios T, Malizos K, Dailiana Z. Midterm experience of Scarf osteotomy as a new technique in a General Orthopaedic Department. Foot (Edinb) 2019; 40: 68-75.
- Law GW, Tay KS, Lim JWS, Zhang KT, Seng C, Yeo NEM, Koo K, Rikhraj IS. Effect of Severity of Deformity on Clinical Outcomes of Scarf Osteotomies. Foot Ankle Int 2020; 41: 705-713.
- Veracruz-Galvez E, Perez-Aznar A, Lizaur-Utrilla A, Lopez-Prats FA, Vizcaya-Moreno MF. Influence of sesamoid position after scarf osteotomy for hallux valgus on patient-reported outcome. A prospective cohort study. Foot Ankle Surg 2022; 28: 471-475.
- Xie W, Lu H, Zhan S, Li G, Yuan Y, Xu H. A Better Treatment for Moderate to Severe Hallux Valgus: Scarf + Akin Osteotomy Combined with Lateral Soft Tissue Release in a Single Medial Incision. Orthop Surg 2022; 14: 2633-2640.
- Bernasconi A, Rizzo M, Izzo A, Vallefuoco S, Russo AP, Rossi V, Abate B, Guarino A, Mariconda M. Bösch osteotomy for hallux valgus correction: results at a mean 10-year follow-up. Arch Orthop Trauma Surg 2023; 143: 1293-1300.
- Izzo A, Vallefuoco S, Basso MA, Ray R, Smeraglia F, Cozzolino A, Mariconda M, Bernasconi A. Role of lateral soft tissue release in percutaneous hallux valgus surgery: a systematic review and meta-analysis of the literature. Arch Orthop Trauma Surg 2023; 143: 3997-4007.
To cite this article
Does the number of screws to fix scarf osteotomy influence the radiographic outcome and the complication rate in hallux valgus? A proportional meta-analysis and systematic review
JOINTS 2023;
1: e812
DOI: 10.26355/joints_202312_812
Publication History
Submission date: 02 Oct 2023
Revised on: 30 Oct 2023
Accepted on: 28 Nov 2023
Published online: 14 Dec 2023