JOINTS 2024;
2: e968
DOI: 10.26355/joints_20245_968
Massive metallosis after medial unicompartmental knee arthroplasty misplacement
Topic: Knee
Category: Case report
Abstract
BACKGROUND: Metallosis is the infiltration of metallic wear debris into the periprosthetic structures. It is a rare complication following joint arthroplasty that may lead to osteolysis, tissue necrosis, pseudotumor formation, cardiomyopathy, or neuropathy. It usually requires surgical treatment, which includes joint debridement and a one or two-stage revision arthroplasty.
CASE REPORT: We report the case of a patient who developed severe metallosis of the knee joint resulting from the secondary friction wear of both the femoral and tibial components of a unicompartmental knee arthroplasty due to malposition and consequent severe wear of the polyethylene insert. The mechanical failure was diagnosed one year after implantation, and metallosis became evident six months later. The patient was treated with a mass excision, extensive debridement, and a single-stage revision with a constrained total knee arthroplasty.
CONCLUSIONS: This case showed the importance of relative prosthetic components position in unicompartmental knee arthroplasty: an incorrect alignment may lead to a severe liner wear and massive metallosis, requiring a prompt extensive joint debridement and prosthesis revision.
Background
Metallosis is a term used to describe the infiltration of metallic wear debris into the periprosthetic structures, including soft and bony tissues. It represents an uncommon condition that can lead to osteolysis, tissue necrosis, and formation of pseudotumors, as well as cardiomyopathy or neuropathy1. Due to the variety of presenting and unspecific complaints, diagnostic and therapeutic management may represent a challenge for the orthopedic surgeon2. The first-line imaging modality is a simple radiography. Three typical signs on X-rays are usually found: the “cloud sign,” characterized by periprosthetic amorphous densities; the “metal line sign,” as a thin hyperdense suprasellar line; and the “bubble sign,” as curvilinear radio intensities outlining the entire joint3,4. Narrowing or asymmetry of the joint space in comparison to previous imaging may be a marker of polyethylene wear5. Other complementary tests include serum laboratory studies (white blood cell count, C-reactive protein, erythrocyte sedimentation rate) and synovial fluid analysis4. Intraoperative cultures are also needed to rule out periprosthetic infection. Common surgical treatments involve debridement, synovectomy, removal of the metallic debris, and one or two-stage revision arthroplasty1.
We report a case of massive wear of the polyethylene of a medial unicompartmental knee arthroplasty (UKA) that produced metal-on-metal abrasion between the femoral and metal-backed tibial components, leading to the formation of metallic debris extended in the periprosthetic soft and bone tissues.
Case Presentation
A 65-year-old man with osteoarthritis of the medial compartment of the right knee received a primary cemented UKA (Journey II Oxinium®, Smith&Nephew, Memphis, TN, USA) at a different hospital in February 2021 without any early complications. Pre-operatively, the patient reported pain localized on the medial compartment (Figure 1). At the physical examination, the knee was stable, and the range of movement (ROM) was 0°-120°; his body mass index (BMI) was 26.
Figure 1. Pre-operative radiograms: right knee osteoarthritis prominent to the medial compartment (2021).

The patient was never satisfied with the results of the surgery, and in April 2021, 6 weeks after the implantation of the UKA, he complained about persistent right knee pain, swelling, and disability. At the examination and blood tests, no signs of infection were found. Early postoperative radiographs showed malposition of the UKA, with a valgus and too lateral tibial component (Figure 2).
Figure 2. Post-operative radiograms after primary unicompartmental arthroplasty: the tibial component is placed in valgus and lateral (2021).
The patient underwent one year of rehabilitation therapies with no improvement of his symptoms, and in May 2022, he presented to our hospital because of increasing pain and disability for the last 4 months. The physical examination showed intact skin, a swollen joint with a range of motion of 10°-100°, and diffuse pain over the medial compartment; neither anteroposterior nor medial-lateral instability was found. There was no localized erythema, increased temperature, or wound discharge that could suggest a prosthetic infection or skin pigmentation. New radiographs demonstrated misplacement of the components with poly wear and some metal debris at the joint line that were not noticed in the beginning (Figure 3). A one-stage UKA to total knee arthroplasty (TKA) revision was then advised.
Figure 3. One year after primary unicompartmental arthroplasty radiograms: little metal debris between the prosthesis components was present (2022).

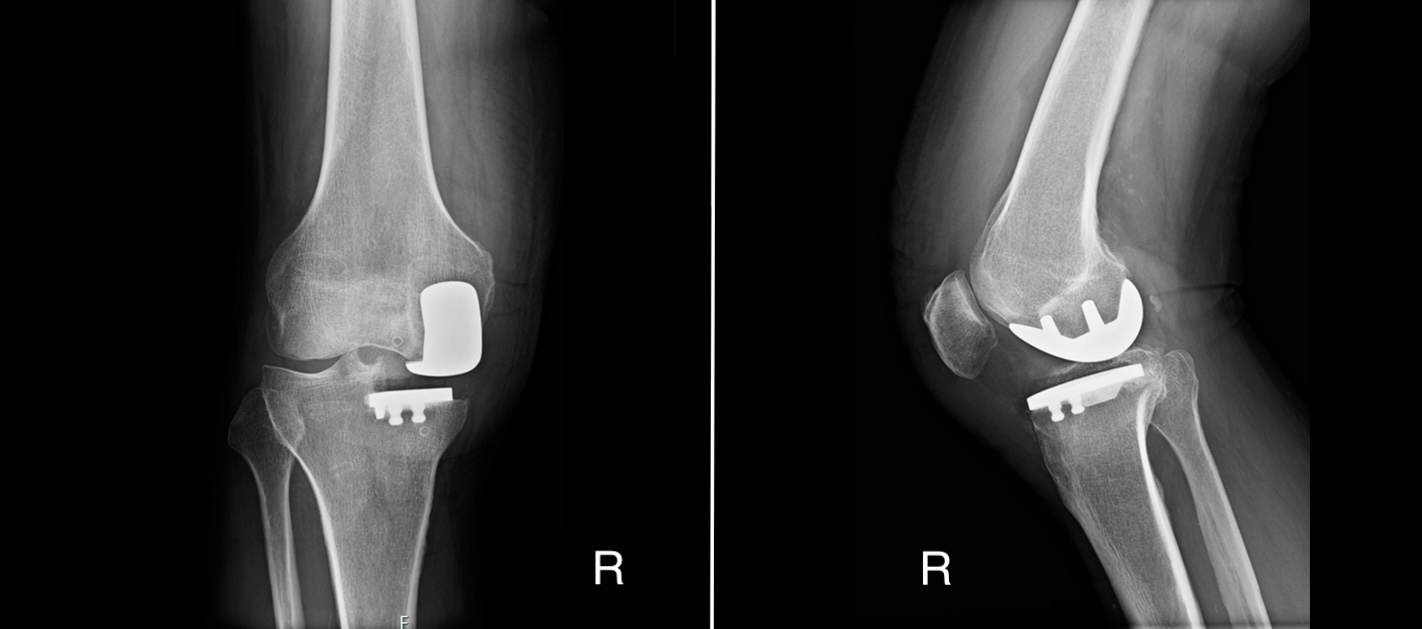
Ten months later, in March 2023, the patient underwent a pre-admission examination. His right knee was still swollen, with a massive popliteal Baker cyst; the ROM was limited to 10-90° and he complained of medial compartment pain. The patient presented no anesthesiologic contraindication to surgery. The results of blood tests were: C-reactive protein (CRP) 1.86 mg/dl, erythrocyte sedimentation rate (ESR) 26 mm/h, white blood cells (WBC) 10. 56×103/μl, neutrophils 75%. The pre-surgery protocol included a standing long X-ray of lower limbs, standard anteroposterior (AP) and lateral right knee X-rays, and Patella Merchant view, which showed massive amorphous densities in the popliteal fossa and the suprapatellar pouch, other than around the prosthesis (Figure 4).
Figure 4. Two years after primary surgery (pre-admission) radiograms: massive metallosis of the right knee with radiographic “bubble sign” (March 2023).

In addition, a magnetic resonance (MRI) and computed tomography (CT) scan with and without contrast medium were performed with the aim of ruling out the diagnosis between metallosis, chondromatosis and infection. From the radiological report emerged “Evidence of distension of the anterior capsular, the anterior recess and the gastrocnemius-semimembranosus bursa with atypical aberrant hyperplastic phenomena; poly wear and subluxation of the prosthesis with depression of the tibial component.” (Figures 5 and 6). The patient reported previous atopic reactions to metal contact, so atopy patch tests for metals were performed, and they were negative.
Figure 5. Pre-admission CT scan and MRI: effusion, polyethylene wear, atypical aberrant hyperplastic phenomena compatible with metallosis (June 2023).
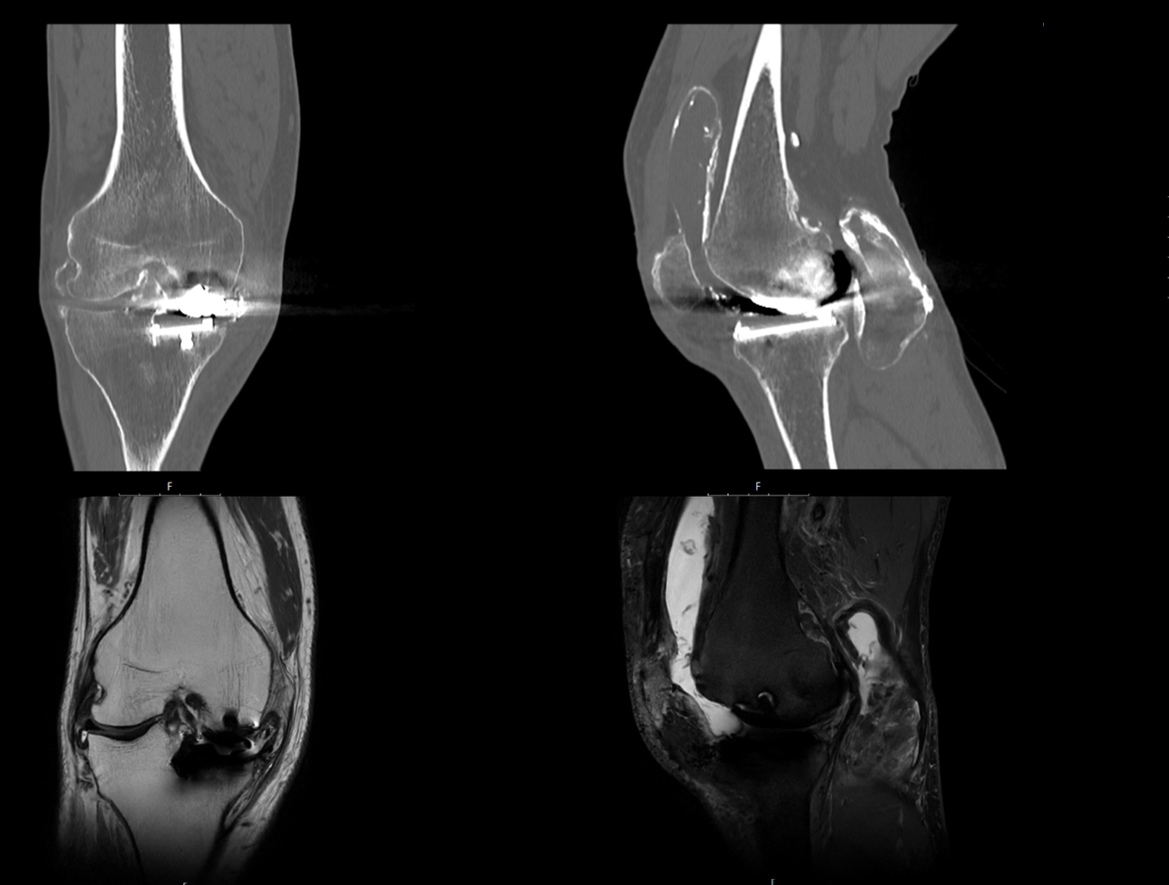
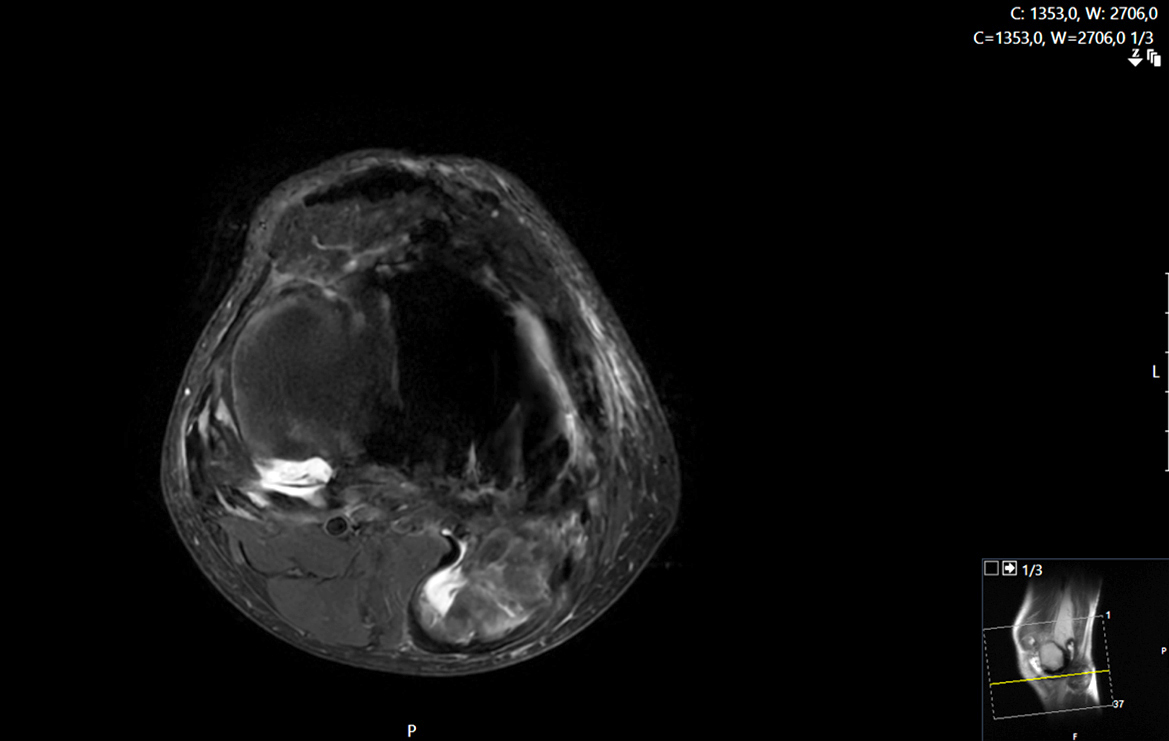
Figure 6. Pre-admission MRI: axial scan evidenced that metallosis posterior mass was medial and far from the popliteal neuro-vascular bundle (May 2023).
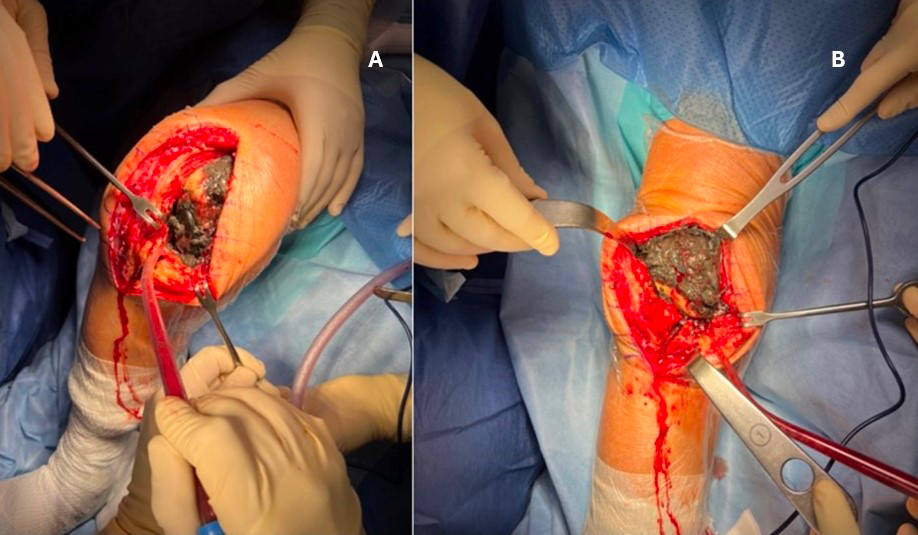
Surgery was performed in June 2023. At the time of admission, new blood tests were obtained, revealing an improvement in the inflammatory markers compared to those taken three months earlier (CRP 0.89 mg/dl, ESR 7 mm/h, WBC 7.74×103/μl). The surgical planning included the removal of the popliteal mass and one or two-stage revision of the UKA with a hypoallergenic total knee arthroplasty based on the results of intra-operative synovial fluid tests. Firstly, the patient was positioned prone, and a tourniquet was applied to the thigh. A posterior approach to the knee was used to remove the posterior capsule and the pseudo-tumor in “one block” (Figure 7). The excised tissue appeared soft and elastic with some gelatinous portions. The mass was capsulated and localized medial to the neurovascular bundle, so no issues were found in approaching and excising it.
Figure 7. Intra-operative pictures. The posterior approach reveals a popliteal capsuled mass (A) that was excised in “one block” (B). The mass section shows a black and amorphous content (C).

Secondly, in the supine position, an anterior medial parapatellar approach was performed, and multiple samples of synovial fluid were collected for intraoperative spot tests (leukocyte esterase and WBC count) in order to rule out infection. A severe synovitis associated with massive metallosis was noticed, while the tibial and femoral components were well fixed (Figure 8).
Figure 8. Intra-operative pictures. Anterior approach: massive metallosis around the prosthesis (A) and in the suprapatellar recess (B).
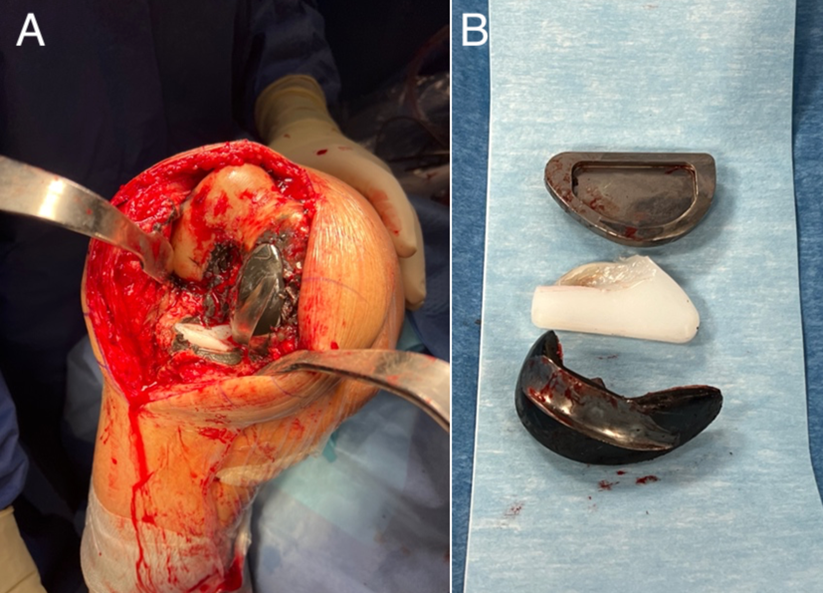
The polyethylene tibial insert showed severe wear that had caused secondary friction between the femoral and tibial metal surfaces, with subsequent macroscopically severe abrasion of the femoral component (Figure 9). The implant and residual cement were removed, and the periprosthetic tissue affected by the metallic debris was debrided. However, a complete removal of metallic particles was not possible. The removed material was sent for histological analysis, while multiple tissue samples were collected for culture.
Figure 9. Intra-operative view of the prosthesis components in situ (A) and after removal (B): no aseptic loosening was found, but there was severe polyethylene and femoral component wear.
The results of the intraoperative spot tests for leukocyte esterase and WBC were negative, so a one-stage TKA conversion was carried out. The bone loss following the UKA removal procedure and the extensive debridement of both bone and soft tissues affected by metallosis lead to the need for a revision system instead of a primary total arthroplasty. Finally, a nickel-free cemented condylar-constrained total knee arthroplasty was implanted (Genus®, Adler Ortho, Cormano, Milan, Italy); the patella was also resurfaced, and the tibial bony defect was filled with cement (Figure 10). A drain was applied, and the wound was sutured with no tension.
Figure 10. Post-operative radiograms: the revision TKA is well placed but some residual postero-medial metallosis is present because of the complexity of displaying and removing it during surgical debridement (June 2023).

Bacteriological cultures of the articular joint fluid did not show any growth. Histological examination confirmed the presence of a massive metallosis with necrotic areas.
Antibiotics (cefazolin 2 g iv, 3 times per day) were administered for 6 days until the results of cultures were available. The patient had a satisfactory recovery from the revision surgery: no early complications were reported, and he was able to walk with crutches from the first day post-operatively. He was dismissed one week later with no pain, slight effusion, and a ROM of 0-100°. At the last follow-up, 6 months after the revision surgery, the patient was satisfied with the treatment and could perform his daily activities free of symptoms, showing a good functional and clinical outcome (ROM 0-110°).
Discussion
Metallosis is a rare complication in knee arthroplasty. Indeed, it has been mostly described6 as a cause of failure in hip replacement, especially in metal-on-metal implants, with a 5% estimated incidence. Different causes have been described in the development of metallosis after TKA and UKA. The failure of metal-backed patellar components, which nowadays have been abandoned for all-polyethylene systems, is considered the most common reason (40% of cases), followed by implant components and polyethylene (PE) failure (27-18%), including wear and dislocation1. Additional causes can be traumatic failures (5%), malalignment, or infections (2% of cases both). Occasionally, iron deposits from the saw blades used during surgery may induce metallosis7.
Few cases of metallosis following a unicompartmental knee arthroplasty were reported in literature8-15. Most of them were caused by PE dislocation or wear; one was a traumatic failure11, another one9 was produced by the anterior cruciate ligament rupture, while one10 was found in a periprosthetic joint infection due to a methicillin-resistant Staphylococcus aureus (MRSA) endocarditis. This complication was mainly addressed with debridement and a one-stage conversion to total knee arthroplasty, except for the need for a 2-stage procedure when a chronic infection was detected.
In this case, the progressive friction between the two metal prosthetic surfaces probably produced metal debris which was the cause of the massive metallosis development.
Similarly to the present case, Greco and Berend8 described a massive metallosis after a metal-on-metal articulation due to the insert dislocation in an oxinium medial UKA (Journey UNI, Smith&Nephew, Memphis, TN, USA). In that circumstance, though, a dysfunction of the liner locking mechanism was responsible for the failure, which is rare in fixed-bearing implants. In our patient, instead, the insert was found still locked into the tibial baseplate but extremely worn out despite only one year passed since the primary surgery. Polyethylene wear is usually seen on an average of 8.3 years after a fixed-bearing UKA implantation and is not one of the most common causes of failure, while dislocation of the mobile bearing is far more frequent16.
Indeed, according to a recent review17, the most common causes of medial UKA failure are aseptic loosening and osteoarthritis progression, followed by bearing dislocation, fracture and tibial subsidence. In particular, mechanical failures may be related to changes in the forces acting on the medial and lateral compartments, which are strongly linked to component positioning and joint space differences after surgery.
Chatellard et al18 showed how changes in joint space height, tibial component obliquity, and a divergence between the tibial and femoral components on the coronal plane, decreased medial UKA prosthesis survival, recognizing that the inclination of the prosthesis could play a role in failure.
In the present case, the tibial component appeared to be positioned in valgus and too lateral, leading to an incorrect alignment between the femoral and tibial implants. Due to the malalignment of the two components, the point of contact was reduced to only a small area where the load was concentrated. Therefore, the asymmetrical prosthetic joint space may have induced premature tibial component wear and, finally, poly breakage, which gradually led to both femoral and tibial metal wear and the spread of debris.
The time period between primary knee replacement and metallosis emergence is usually reported as several years1. At initial presentation, symptoms are not specific in most of the cases, including pain, swelling and restricted range of motion of the affected joint. The physical examination shows a joint effusion and sometimes crepitus or ligamentous instabilities; in our case, no specific signs such as skin discoloration, a fistula, or friction noises induced by metal-on-metal contact were present; therefore, a diagnosis of metallosis was difficult to think of in the beginning, and the revision surgery was planned with no urgency. Interestingly, one year before the huge mass was noticeable on radiographs, the patient presented only a few tiny signs of debris in the joint space that were not highlighted by either the radiologist or the orthopedic surgeon. The voluminous metallosis mass developed in the following few months while waiting for the revision surgery. In addition, the severe wear of the fixed bearing was not appreciated in the beginning, maybe due to the lack of a metal marker within the polyethylene insert. For all these reasons, in the present case, diagnosis and treatment were delayed. As reported by Schiavone Panni et al13, metallic debris is not biologically inert, but it activates the inflammatory cells, which release cytokines leading to chronic synovitis, osteoclastic bone reabsorption, and osteolysis; moreover, because of the rich vascularization of the synovial membrane, metallic debris tend to deposit inside the vessels and consequently spread to lymph nodes and other organs, such as spleen, lungs and liver. Therefore, metallosis should be diagnosed in its early development, and it is advisable to perform a synovectomy with revision surgery as soon as possible.
Some studies8,9,19 analyzed the presence of metal-nickel and cobalt allergies in patients who presented with metallosis after knee arthroplasty. One author19 supposed the patient’s allergy status contributed to the metallosis. This condition involves chronic inflammatory arthritis caused by metal hypersensitivity, particle-induced synovitis, and the toxic effects of the metal particles. In our case, a nickel-free prosthesis was used for revision because of a positive history of metal atopic reaction despite the negative results of pre-operative patch tests. In fact, this kind of diagnostic procedure is known to produce false negative results in some patients, such as in cases of insufficient exposure time, a patient’s low sensitivity to certain allergens, or previous treatments and medications that interfere with the reaction.
Conclusions
The described case showed the importance of relative prosthetic components’ position in unicompartmental knee arthroplasty. An incorrect alignment may lead to severe liner wear and massive metallosis in a few months, requiring extensive joint debridement. A metallosis, though rare, should always be considered in case of implant failure, and in that case, an early revision surgery should be planned.
Conflict of Interest
The authors declare that they have no conflict of interest to disclose.
Informed Consent
Written informed consent was provided by the patient for permission to receive therapy and to publish this case report.
Ethics Approval
Not applicable since data were collected as part of routine care.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Authors’ Contributions
D’Anchise Roberto: responsible for surgical treatment and analysis of imaging and data for the described case, other than validating the final paper.
Ricci Martina: collaborated on writing the introduction, case presentation and discussion of the present paper and collecting data for the present case.
Impieri Lorenzo: collaborated on writing the introduction and case presentation, collecting data, and formatting figures and references.
Balbino Cristiana: responsible for paper review and literature research.
Manta Nicola: collaborated on writing, discussing, and reviewing the paper.
ORCID ID
Ricci Martina: 0000-0003-1107-9298
Impieri Lorenzo: 0000-0003-1975-3670
Funding
The study was not supported by any source of funding.
References
[1] Sahan I, Anagnostakos K. Metallosis after knee replacement: a review. Arch Orthop Trauma Surg 2020; 140: 1791-1808.
[2] Salem KH, Lindner N, Tingart M, Elmoghazy AD. Severe metallosis-related osteolysis as a cause of failure after total knee replacement. J Clin Orthop Trauma 2020; 11: 165-170.
[3] La Verde L, Fenga D, Spinelli MS, Campo FR, Florio M, Rosa MA. Catastrophic metallosis after tumoral knee prosthesis failure: A case report. Int J Surg Case Rep 2017; 30: 9-12.
[4] Mallon S, Bussis K, Beswick Z, North WT, Soliman SB. Ultrasonographic and radiographic findings of polyethylene component displacement with severe metallosis and metal-induced synovitis following total knee arthroplasty. Knee 2019; 26: 941-950.
[5] Anderson JA, MacDessi SJ, Della Valle AG. Spontaneous, Recurrent Dislodgment of the Polyethylene Tibial Insert After Total Knee Arthroplasty. J Bone Joint Surg 2007; 89: 404-407.
[6] Oliveira CA, Candelária IS, Oliveira PB, Figueiredo A, Caseiro-Alves F. Metallosis: A diagnosis not only in patients with metal-on-metal prostheses. Eur J Radiol Open 2015; 2: 3-6.
[7] Klontz KC, Smith WI, Jonathan CK. Acute Metallosis Following Total Knee Replacement – A Case Report. J Orthop Case Rep 2014; 4: 21-23.
[8] Greco N, Berend K. Polyethylene liner dislocation of fixed-bearing medial oxinium unicompartmental arthroplasty with severe metallosis. Knee 2018; 25: 341-345.
[9] Rajgopal A, Panda I, Tyagi VC. Early failure with massive metallosis and posteromedial wear following atraumatic anterior cruciate ligament rupture after medial unicompartmental knee arthroplasty. Arthroplast Today 2017; 4: 15-19.
[10] Alayane A, Moussa MK, Boushnak MO, Boulazaib I, Nicolas N. Septic Metallosis after Unicompartmental Knee Replacement: A Case Report and Literature Review. J Orthop Case Rep 2023; 13: 11-15.
[11] Sanchis-Alfonso V. Severe metallosis after unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2007; 15: 361-364.
[12] Luyet A, Fischer JF, Jolles BM, Lunebourg A. Unexpected wear of an unicompartimental knee arthroplasty in oxidized zirconium. Acta Orthop Belg 2015; 81: 790-795.
[13] Schiavone Panni A, Vasso M, Cerciello S, Maccauro G. Metallosis following knee arthroplasty: a histological and immunohistochemical study. Int J Immunopathol Pharmacol 2011; 24: 711-719.
[14] Apostolopoulos AP, Katsougrakis I, Fanous R, Harrison A, Saavedra E. Severe metallosis following polyethylene dislocation in a mobile-bearing medial unicompartmental knee replacement. J Long Term Eff Med Implants 2014; 24: 147-150.
[15] Vecchini E, Ditta A, Gelmini M, Maluta T, Valentini R, Ricci M, Magnan B. Rupture of the femoral component and severe metallosis of the knee 10 years after unicompartmental knee arthroplasty (UKA): a case report. Acta Biomed 2019; 10: 198-202.
[16] Kim KT, Lee S, Lee JI, Kim JW. Analysis and Treatment of Complications after Unicompartmental Knee Arthroplasty.Knee Surg Relat Res 2016; 28: 46-54.
[17] Tay ML, McGlashan SR, Monk AP, Young SW. Revision indications for medial unicompartmental knee arthroplasty: a systematic review. Arch Orthop Trauma Surg 2022; 142: 301-314.
[18] Chatellard R, Sauleau V, Colmar M, Robert H, Raynaud G, Brilhault J. Medial unicompartmental knee arthroplasty: Does tibial component position influence clinical outcomes and arthroplasty survival? Orthop Traumatol Surg Res 2013; 99: 219-225.
[19] Vivegananthan B, Shah R, Karuppiah AS, Karuppiah SV. Metallosis in a total knee arthroplasty. BMJ Case Rep 2014; 2014: bcr2013202801.
To cite this article
Massive metallosis after medial unicompartmental knee arthroplasty misplacement
JOINTS 2024;
2: e968
DOI: 10.26355/joints_20245_968
Publication History
Submission date: 05 Feb 2024
Revised on: 12 Mar 2024
Accepted on: 15 Apr 2024
Published online: 30 May 2024